
For nearly a century now, we thought we knew what the essential fatty acids were, linolenic acid and alpha-linoleic acid. I’ve written it in my books and in various articles as have many others. As so often happens in science, with new data comes new models. Because it looks like we may have been wrong about what the real essential fats are. As always, let me start with some background.
Table of Contents
What is an Essential Nutrient?
Before discussing what the essential fats are or may be, I need to make sure everybody is clear on what an essential nutrient is. Now, this can get confusing since technically there are two different types of nutrient essentiality: physiological and nutritional.
- Physiological essentiality means a nutrient is essential for life.
- Nutritional essentiality means that nutrient is essential in the diet because the body can’t make it or can’t make enough of it.
I’ve provided the full criteria for an essential nutrient below.
Vitamin C is one example. Unlike some animals who can make Vitamin C, humans cannot. If Vitamin C intake is absent or insufficient, characteristic signs of deficiency, disease (i.e. scurvy) and eventually death occur. Replacing Vitamin C in the diet (i.e. citrus fruits to sailors back in the day) correct it. Hence Vitamin C is nutritionally essential and must be obtained in the diet.
In contrast is something like dietary cholesterol. While it is physiologically essential, it can be made by the body in sufficient amounts. Hence is is not nutritionally essential and is not considered an essential nutrient.
Related: What Is the Difference Between Dietary Fat and Cholesterol?
Similarly, about half of the amino acids are essential and half are non-essential (or inessential). The essential amino acids can’t be made by the body (or can’t be made in sufficient amounts) while the non-essential amino acids can be made in the body from other amino acids. This ends up being fairly moot since effectively all dietary proteins contain all of the amino acids. But athletes occasionally get hung up on Essential Amino Acid (EAA) supplement which only contain the half or so which are essential.
For completeness, I should mention the concept of conditional essentiality. This refers to a nutrient that is normally not nutritionally essential but which may become so under specific conditions. That is, under normal circumstances the body can make enough but, under abnormal circumstances it cannot do so. Typically those are related to various disease states, pathologies or with certain genetic defects but there are exceptions.
Vitamin D is one. While usually considered an essential nutrient (i.e. it must come from the diet), it is more likely to be conditionally essential since it is generated by the body via sun exposure. So long as someone gets sufficient sun, they do not need to get Vitamin D from the diet. If they don’t get enough sun, they do.
I’ll mention another below.
What are the Essential Nutrients?
Over a century plus of nutritional research, the essential nutrients have been fairly well established. They include water, energy (calories), the essential amino acids along with a laundry list of vitamins, minerals and ultra-trace minerals. And there are still a few being hashed out/debated even now.
Related: What Are Calories?
You’d note that I didn’t put carbohydrates on that list and technically they are not an essential nutrient. Under even zero-carbohydrate intakes, the body can make what little carbohydrate it needs from other sources such as lactate, glycerol and some amino acids. Since most of the body’s metabolism shifts to using fat for energy anyhow, the total requirement for carbohydrate is pretty low.
At the same time, I would argue that carbohydrate become conditionally essential if someone is performing lots of high-intensity activity. Under that condition, the body cannot make sufficient glucose to maintain muscle glycogen and fuel the exercise. We might also quibble over digestible carbohydrates versus fiber in terms of what is essential but I’m getting off track.
But what about dietary fats? Are they essential? Or rather are there essential dietary fats? The short answer is yes there are two essential fatty acids (hereafter EFAs). Traditionally we’ve always thought we knew which two were the EFAs that had to come from the diet.
And as you might guess the point of this article is to bring up data suggesting that that long-held belief may not be correct.
A Primer on Dietary Fats
Once again for background, let me do a quick run through of the types of dietary fats. The names refer to their chemical structure and I’d point you elsewhere for a more detailed discussion.
Trans-Fats (TFA): While there are naturally occurring TFAs, usually the term refers to fats made by bubbling hydrogen through unsaturated fats to make them more shelf stable. TFAs are not required by the body, are not essential and, in fact, most feel that they have no place in the diet at all. It’s one of the very few places in nutrition where basically everybody is in agreement.
Saturated Fats (SFA): Saturated fats are a class of fats which are related by chemical structure. They are found almost exclusively in animal food products (exceptions are coconut and palm kernel oil) and are solid at room temperature. They aren’t essential nutritionally or physiologically. If you never ate another gram, you’d be fine. That’s not a recommendation, by the way, just a statement of physiological reality.
Unsaturated Fats: The unsaturated fats technically encompass two sub-categories. The first are mono-unsaturated fats (MUFA) the most well known of which is oleic acid, found in olive oil. While healthy, oleic acid is not essential nutritionally or physiologically. The second are the polyunsaturated fats (PUFAs) which are sometimes referred to as w-3 (or n-3 or omega-3) and w-6 (or n-6 or omega-6) fatty acids. The nomenclature refers to their chemical structure (MUFA are w-9/omega-9 for the record).
And it is the w-3 and w-6 PUFA that are the essential fats. Well, kind of. By which I mean I have to get into more details.
Will the Real Essential Fatty Acids Please Stand Up?
While certain types of science seem relatively easy to do in the modern era, it’s important to realize that this wasn’t always the case. In terms of the essential nutrients, most of the work was being done in the early part of the 20th century and it often took a lot of work to determine if a nutrient was truly essential or not.
Predominantly what was involved was deliberately creating a nutrient deficiency for long enough that a distinct symptom or set of symptoms would show up. Then that nutrient would be provided again to see if it made the problem go away. Ideally the rest of the diet was completely controlled.
While this was relatively easy to do in rats and mice, it’s critical to realize that nutrient requirements between species differ. Eventually you had to do it in humans and this wasn’t always easy since it was tough to control. From memory, they often used prison or military populations but don’t swear me to that. I recall one story of a researcher and his wife who put themselves on a nutrient deficient diet to prove that it was essential because nobody else believed them. Early science was mental.
In the case of dietary fats, it actually took many years to even demonstrate that there were essential fatty acids (EFAs). Simply, nobody could seem to create a severe enough deficiency for symptoms to appear. Even in early animal studies, the lowest of fat intakes seemed to prevent deficiency prompting one early research to conclude:
“If true fats are essential for nutrition during growth the minimum necessary must be exceedingly small.” (ref. 17; p. 152)
It provided a real problem in a scientific sense.
So how did they finally do it?
EFA Requirements in Animals
In animals, literally zero fat diets would do it and this would lead to the early identification of linoleic acid (w-6) as an EFA in 1930. Followup studies would further find that arachidonic acid (AA) a metabolite of linoleic acid was also essential. Keep that in mind.
Similar work would eventually determine that alpha-linolenic acid (w-3) was essential in rats although there was great controversy for reasons too boring to detail here. One indicator suggesting that ALA was essential was the discovery that EPA and DHA (often referred to as the fish oils and don’t worry what they are abbreviations of), metabolites of ALA played their own important role in the body. Keep this in mind too.
EFA Requirements in Humans
If determining the existence of EFAs in animal models was tough, it was damn near impossible in humans. There was some early indication in the 1930’s that there might be essential. The same basic reason held: even the lowest fat intakes would prevent gross deficiency symptoms from occurring. As above, if there was a dietary requirement, it was tiny. And if you couldn’t create a deficiency to begin with, you couldn’t establish essentiality in a nutritional or scientific sense.
For decades, it was unclear if humans had a true EFA requirement and this wouldn’t really change until 1968, decades after the initial discovery. At this time, something called total parenteral nutrition (TPN) was developed. TPN is used to provide nutrients via infusion rather than oral intake. And early formulations were completely fat free.
And it was at this point that humans started to show EFA deficiencies. Which were found to be reversed by the addition of LA and ALA. Boom, these were determined to be the essential fatty acids, required in the diet in, admittedly small amounts (something like 1-2% of total dietary intake). Both were shown to be essential by selectively providing one or the other and showing that they weren’t interchangeable.
To that I’d add that the importance of EPA and DHA came to light with the observation in the 1970’s that the Alaskan Inuit had extreme low levels of heart disease which seemed to be related to their high intake of those specific fats (hence called the fish oils due to their high presence in fatty fish).
But ultimately it had been determined that humans did have an essential fatty acid requirement. And for decades the traditionally held view was that the EFAs were LA and ALA. Nutrition textbooks list LA and ALA as the EFA’s, I’ve done the same in my books and articles and so does everybody else.
But is this actually the case? Are LA and ALA the real essential fatty acids?
You can probably guess that there’s more to it or I wouldn’t bother writing this article.
To understand why they might not be, I need to look at some more boring biochemistry.
ALA and LA as Precursors to Other Molecules
Most things in the body under go significant metabolism after ingestion. Dietary starches are broken down to glucose which can be used for energy or stored as liver or muscle glycogen. Dietary proteins are broken down to individual amino acid chains and those AAs can be used for tissue rebuilding, burned for energy, converted to ketones along with other metabolic fates.
Dietary fats are no different. The unsaturated fatty acids specifically undergo a great deal of metabolism in the body with scary sounding chemical processes like desaturation and elongation occurring to produce other related chemical compounds. Those other compounds often playing as if not more important roles in the body than the parent molecule.
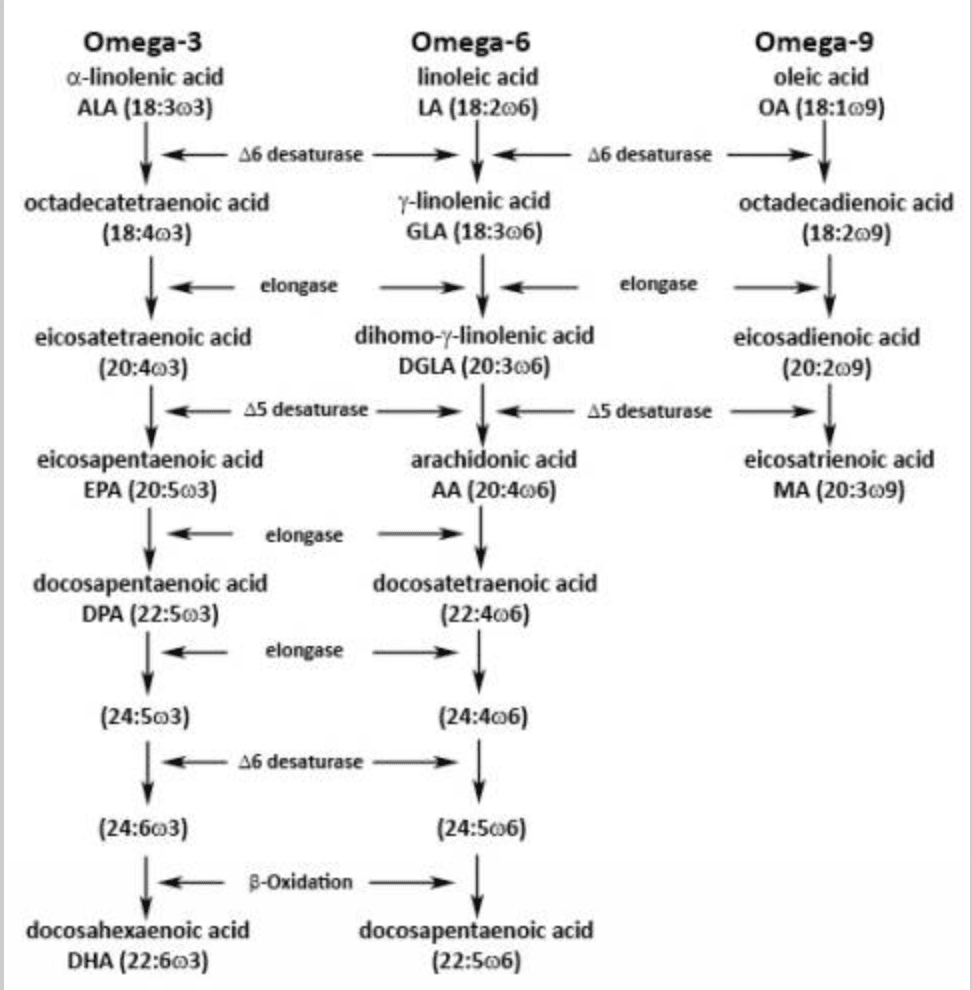
Here’s a chart showing the chemical transformations that occur for the w/omega-3 (alpha-linolenic), w/omega-6 (linoleic acid) and w/omega-9 (oleic acid) fatty acids. No, omega-9 is not essential. It’s simply in the chart and there can be limited interconversion to other compounds so it’s worth showing.
So you can see in the chart that, as I mentioned above alpha-linolenic acid eventually converts to EPA and DHA while linoleic acid converts to AA. In addition to many other roles in the body (i.e. activating PPARs and gene expression, being incorporated into cell structure), those can be converted to eicosanoids, short lived chemical messenger that do tons of stuff in the body.
Some of these deal with inflammation and much is often made of the fact that AA tends to generate inflammatory eicosanoids and EPA/DHA generate anti-inflammatory eicosanoids. Much is then made of the ratio of w-6:w-3 fatty acids in the diet with excessive ratios being potentially problematic. I’ve discussed this elsewhere and won’t get into the details here. I’ll only note that the modern diet tends to be very high in w-6 fat sources and very low in w-3 fat sources by and large.
It’s even more confusing because, as you can see in the chart, the fatty acids all use the same enzymes. If you have too much of one fatty acid, it ends up monopolizing that enzyme and you don’t get optimal metabolism of the other fatty acid. So if you have too much w-6 in the diet, whatever w-3 you are consuming isn’t being optimally converted to EPA/DHA.
Determining the Real Essential Fatty Acids
The take home point of the above is simply this: LA and ALA are converted to downstream metabolites such as AA and EPA/DHA respectively. And AA and EPA/DHA are known to play important physiological roles in the body.
This raises the basic question of whether LA and ALA are the true essential fatty acids or whether they are simply precursors to the compounds which really matter and are, by definition, truly essential.
The answer to this essentially hinges on two different issues:
- Does the parent fatty acid have any essential role outside of conversion to its metabolite?
- Does consumption of the parent fatty acid provide enough of the “essential” metabolite?
Looking at number one, it’s entirely possible that something like LA or ALA would have its own metabolic effects in the body in addition to its conversion to AA or EPA/DHA respectively. Determining this can be a real hassle scientifically since you’d have to find a way to test LA/ALA while inhibiting downstream conversion. I’ll be honest that I skated on researching this and won’t go into much detail. However, in the big picture only one paper I looked at even briefly mentioned a direct physiological role of LA.
Number two is a little bit more important in my mind. We know that AA and EPA/DHA play critically essential roles in the body. That even if those effects occur in addition to the effects of the parent fatty acids, they are critical to human health and function. They can be considered “essential” fatty acids even if their essentiality is in addition to their parent fatty acids.
But it’s equally possible that AA and EPA/DHA are essential and LA/ALA are not.
Now this might seem like semantic irrelevancy in the big picture. Whether or not LA/ALA or their metabolites is essential doesn’t really matter so long as LA/ALA intake produce sufficient amounts of those metabolites.
Either way you get enough of the “essential nutrient”, right?
But this assumes that consuming just the parent compound does in fact produce enough of the “possibly” more essential metabolites.
So do they?
Metabolism of LA to AA
Ok, let me get the easy one out of the way first which is LA and AA. Honestly, different papers report different things here in terms of whether or not the conversion of LA to AA is sufficient to meet daily requirements.
Based on an indirect marker I won’t try to explain, one paper on the topic states that the large intake of LA in the Western diet means that there is always sufficient amounts of AA being produced. I’d also note that despite being “essential” fat cells are about 10% LA to begin with. It is stored within the body and is released into the body during a calorie deficit. I’ll also note that this is NOT the case for LA or the w-3’s.
In contrast, another review found that tissue levels of AA change only minimally with enormous changes in LA intake from high to low. In contrast, supplementing GLA (gamma linoleic acid, two steps above AA in the char above) or AA itself does impact tissue levels (whether or not this is a good thing or bad thing is a separate issue).
They conclude that the conversion is limited enzymatically and point out that the conversion of LA to AA occurs at an efficiency of only 0.3-0.6%. This still doesn’t really answer the question of whether LA or AA is essential since that might still provide enough to meet the body’s needs. Which doesn’t change the fact that AA seems to be “essential” in the sense of the nutrient that is actually important to the body.
Note: The seeming contradiction probably has to do with differences in the measured endpoints. If you’re looking at the amount of AA in the bloodstream, LA intake may be sufficient. If you’re looking at changing tissue levels of AA, it may not be. No, I’m not getting into this any deeper.
Beyond that, this seems to be a question without a solid answer at least in humans. In animal models at least, simply providing AA will reverse deficiency symptoms similarly to LA. This indirectly suggests two things
- LA is not essential in and of itself.
- LA acts as no more than a precursor compound and that AA is the truly essential fatty acid.
Put differently: you could ignore LA completely and just consume AA and be fine because it is the real essential fatty acid.
Let me note that I’m not a fan of animal research since it rarely if ever translates directly to humans.
For what it’s worth, the World Health Organization (WHO) recommends that AA be added to infant formula. But this might just be because infants don’t convert LA to AA. Or simply that the nursing mother does the conversion in her body to begin with.
AA has also been shown to improve various types of neurological function. Similarly, AA supplementation was popular years ago since it was shown to be ergogenic something that has not been shown for LA for the most part. But this only points out that AA is important physiologically, not whether it’s more essential than LA or the truly essential w-6 fatty acid . I’ll come back to this when I wrap up.
Metabolism of ALA to EPA/DHA
And now let’s look at the issue of ALA and its conversion to EPA/DHA. As I mentioned above, observations of the Alaskan Inuit in the late 70’s really brought the importance of EPA/DHA to light indicating that they had enormous direct physiological roles in the body.
The short version is this: despite a very high-fat diet, the Inuit showed low levels of heart disease. And this was thought/found to be due to the enormous intake of EPA/DHA, found in fatty fish and giving them their more common name of “fish oils”.
Initially EPA was thought to do the heavy lifting in terms of heart disease for more boring physiological reasons. Soon thereafter the (arguably more) critical importance of DHA in the body came to light. DHA plays many critical roles in human physiology throughout the lifespan not the least of which is in neurological function.
DHA is the primary structural fat in the brain and providing sufficient DHA during fetal growth and childhood improves neurological development. On this topic, if you want to go down a real rabbit hole on the idea that fatty fish may have been critical to human development, check out The Aquatic Ape Hypothesis. It’s dismissed by almost all anthropologists but make for some fun reading.
Pregnant and nursing women have been recommended to get several grams of w-3’s with 100-300 mg per day of DHA specifically to ensure optimal brain development. I’d personally just say get the 1.8-3 grams of combined EPA/DHA I’ve suggested for nearly 15 years now and be done with it as this will readily cover any EPA and DHA requirements.
In any case, that alone suggests that DHA rather than ALA per se might be the essential nutrient.
In that vein, one review concluded that ALA had no impact on numerous markers of cardiovascular health or inflammation per se, both of which are known effects of supplementing EPA/DHA. ALA supplementation also doesn’t seem to be related to changes in biomarkers of EPA/DHA level.
Basically, ALA alone doesn’t seem to have any major impact in and of itself (as noted, no paper I read for this piece suggested an independent biological role for ALA outside of being converted to EPA/DHA). Or certainly not the same effect that is known to occur with EPA/DHA supplementation.
So what’s the problem? Why doesn’t ALA get the job done?
Conversion of ALA to EPA/DHA
And the reason for this is that the conversion of ALA to EPA and DHA are quite poor under most conditions. In men, for example, the conversion of ALA to EPA is about 8% efficient with the conversion to DHA being an almost insignificant 0.1%.
In women the values are better especially the conversion to DHA. Interestingly, this goes up even further during pregnancy with DHA production from ALA increasing further. Given the absolute criticality of DHA for proper fetal brain development this makes sense. Estrogen is assuredly involved and I discussed this to some degree in The Women’s Book Vol 1.
I’ve actually talked about this in several of my books. Years ago when the whole EFA thing broke in the fitness and bodybuilding world, a common suggestion was to consume flax oil, one of the few oils that contains large amounts of ALA.
Unfortunately, flax or other high ALA fat sources are not an ideal solution for the reasons I just stated: the conversion to the key players, EPA/DHA (and possibly DHA only) is too low to make it optimal. I’ve long recommended preformed fish oil supplements for this reason.
Certainly, fatty fish can be consumed instead but in my experience there is a huge cultural aspect to who does and doesn’t like to eat that kind of fish. If you like fatty fish, eat them. If not, take preformed fish oils or get a liquid fish oil like Carlson’s and put it on your salad.
But ultimately consuming ALA itself will only raise EPA levels in the body a little. And it will raise DHA levels almost not at all. Since the effects of critical importance here are related to EPA/DHA per se and possibly to DHA alone, it doesn’t get it done.
Two More Data Points
Before wrapping up, I want to mention two more papers of interest.
AA Spector
The first is a 1999 review on the topic of essential fatty acids. Examining the same biochemical pathways and then some, it makes the two following statements within the body of the paper:
The need for arachidonic acid (20:4n-6) almost certainly is the primary reason why n-6 PUFA are essential.
The use of the word primary is due to it listing a specific role of LA as a part of the skin’s lipid membrane which is about the only independent purpose of LA I’ve seen mentioned. This is the ONLY paper I found that mentioned any independent role of LA in human physiology.
Similarly, it states:
Under ordinary conditions, DHA (22:6n-3) is the most abundant n-3 PUFA contained in the tissues, especially in the brain and retina. For this reason, it seems more likely that DHA rather than EPA is the essential n-3 component.
Surprisingly, I was unable to find any more recent paper addressing the topic in this fashion. But it’s overall conclusion seems consistent with the view that AA and DHA specifically are the truly essential fatty acids with LA possibly having a singular independent role and ALA being nothing more than a precursor fatty acid.
Hau D. Le et al.
The second is the paper that actually stimulated me to write this piece. Ok, that’s not true, it was referenced in a recent paper that talked about essential nutrients and referenced it in terms of debate over what the true essential nutrients actually are.
Titled The essentiality of arachidonic acid and docosahexaenoic it first presents a review of all the topics I discussed above. Following that, it points out the researcher’s clinical experience using total parenteral nutrition (TPN) in a pediatric population.
Yes, I know that this is not necessarily or automatically an applicable population to adult humans. However, inasmuch as EFAs are arguably more important for proper development during childhood, I think it’s relevant.
They describe their use of a fish oil based lipid emulsion in their TPN containing only AA and DHA with insignificant amounts of either LA or ALA.
While concerns had been raised that this might cause problems, not only did they find that it treated some of the issues inherent to TPN, it prevented the development of an EFA deficiency. Simply, the provision of AA and DHA alone were sufficient, lending support to the idea that they and they alone are the true essential fatty acids
So What Are the Real Essential Fatty Acids?
So have I reached a conclusion? Well, sort of. Let’s sum up.
- Some nutrients are essential in that they must come from the diet as the body can’t produce them/produce enough of them.
- Even though it took decades, it was established in humans that there is an essential fatty acid requirement.
- Initially the essential fatty acids were felt to be the w-6 Linoleic acid (LA) and the w-3 alpha-linolenic acid (ALA).
- But as much as anything it looks like those two parent fatty acids exert most of their effect via conversion to the downstream metabolites arachidonic acid (AA) and EPA/DHA. That is, it’s questionable if they play any direct role in and of themselves.
- Where AA and EPA/DHA seem to be the reason for the apparent “essentiality” of the parent LA and ALA fatty acids.
- The conversion of LA to AA may or may not be sufficient depending on what paper you read.
- But it’s very very clear that the conversion of ALA to EPA is low and to DHA is nearly nil.
- One older review states directly that the primary role of LA is to provide AA and that DHA is assuredly the essential compound rather than EPA or ALA.
- Limited clinical evidence suggests that the provision of only AA and DHA in TPN prevents signs and symptoms of essential fatty acid deficiency.
So from the standpoint of providing sufficient amounts of the truly important fatty acids, AA, EPA and DHA, it wouldn’t appear that LA and ALA are ideal to begin with. It’s questionable if they have any independent role in human function outside of being a (relatively) poor parent compound to make what matters.
And this would lead me to conclude that LA and ALA are not truly essential fatty acids. Rather, they only act as (generally poor) precursors for other compounds. LA intake may provide sufficient AA but it’s clear that AA supplementation acts differently. ALA might provide sufficient EPA barely but is inadequate to providing sufficient DHA, the one that really matters.
And I think that overall the data points to AA and DHA being the true essential fatty acids. Future research may confirm or dispute that and I’ll be watching for it. Now we just have to wait for a supplement company to jump on the idea…
Facebook Comments