Since I am fairly open about my own issue with bipolar (specifically Bipolar II, the “lighter” form), I often get questions related to the topic. The one I want to address today was short and do the point: Is bipolar disorder caused by inflammation? Usually the questions are a bit more individually directed by I actually like these.
Because despite the fact that I have bipolar (specifically bipolar II, the lighter form), I don’t really keep up with the developments in it. I’m medicated, I’m stable, I’m happy and, honestly, I have other things on my plate. So questions like this force me to get up my own butt and do some research and learn something new. And in this case I got up my own butt to see if bipolar was in fact and inflammatory condition.
And the short answer is yes-ish.
Now here’s the long answer.
Table of Contents
A Couple of Comments about Inflammation
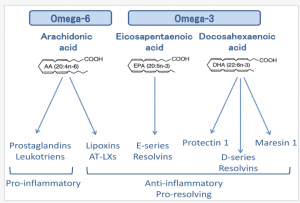
Inflammation has become the new big buzzword in health and, like so many things, tends to carry the connotation of being nothing but a negative. Most of the focus tends to be on the modern diet and whether or not certain components are or aren’t inflammatory to the body with the usual focus being on things like sugar or an excessive omega-6:omega-3 ratio being inflammatory while other foods are anti-inflammatory.
I’ve addressed the omega-6:omega-3 thing previously on the site and will only say that I think parsing out specific parts of the diet in terms of inflammation is a problem for a big reason: obesity is an inflammatory condition in and of itself (fat cells are actually part of the immune system which means that increasing amounts of bodyfat are part of this inflammation).
Which means that, given commonalities in diet that tend to be present in the obese makes it difficult in mind to separate out the impact of the diet from the fact that someone is obese. That said, how studies typically do this is give some dietary component and measure the actual inflammatory response although differences are often seen between lean and obese individuals. I’d be lying if I said I had looked into this in huge detail.
Let me also note that the inflammatory or anti-inflammatory pathways in the body are excruciatingly complicated in terms of how they work. I don’t pretend to be able to detail them and won’t bother. Right or wrong I’ll simply use the terms anti- or pro-inflammatory to indicate whether something decreases or increases inflammation respectively. And with that said.
Bipolar and Inflammation: Part 1
As above, well, kind of. A recent review has examined this issue and concluded that yes, there is evidence of both central (brain) and peripheral (body) inflammation when bipolar is present and that alterations in the immune system are critical to the pathophysiology of bipolar. Elevated levels of pro-inflammatory cytokines (short-lived signalling molecules that may even play a role in overtraining as well) have been found and well, this certainly points to inflammation being involved. Of that there is no doubt.
I’d note in this vein that brain inflammation has also been found to occur in obesity and may be part of the metabolic syndrome (i.e. Syndrome X or whatever the current term for it is) as well. Basically, inflammation in the brain is present in a lot of situations and that often goes hand in hand with inflammation in other parts of the body.
Treating Bipolar Inflammation
In the above vein, it’s worth talking about anti-inflammatory compounds, starting with lithium. Lithium has been the gold standard for bipolar treatment for decades but, given that, nobody actually knows how it works which is a bit surprising when you think about it. A number of mechanisms have been proposed but at least one involves it having anti-inflammatory effects in the brain. Hmmm….
Similarly, while research is a bit mixed, there is at least some evidence that various types of anti-inflammatory drugs such as Non-Steroidal Anti-Inflammatory Drugs (NSAIDs such as aspirin, ibuprofen, etc.), w-3 fish oils, n-acetyl cysteine (NAC) and pioglitazone may improve the effects of other bipolar drugs, at least in bipolar depression. Why it doesn’t impact mania, I have no idea.
Adding to this, I actually ended up having an appointment with my NP between starting and finishing this piece and she told me she had just read a paper on the topic. I mentioned when I talked about my own bipolar that they had given me a genetic test and apparently one of the tests (that I was negative for) indicates issues with inflammation and they use a specific nutrient compound for those people. I have already completely forgotten the name of it, sadly.
Depression per se appears to have an inflammatory aspect and the w-3 fatty acids (specifically the EPA component) have at least a small effect in improving depressive symptoms along with improving some components of the metabolic syndrome. I think you get the idea.
So the case would seem to be closed, a variety of conditions ranging from obesity to metabolic syndrome to depression to bipolar are related somehow to inflammation. I’d mention briefly that many of the comorbid conditions such as coronary artery disease, obesity and insulin resistance, osteoporosis, and pain that occur with bipolar may be related to this same inflammation.
It’s also important to note that in no way is inflammation the only change that occurs in bipolar, it’s simply one that appears to be playing a major role. There are clearly changes in neurochemistry, BDNF (Brain Derived Neurotophic Factor) and the cortisol axis may all be impacted. Multi-factorial is a word I wish more people would tattoo on their foreheads since it’s never just one thing at work in most cases.
So the cure (and this was the gist of the article that I’m not linking to because I’m about to shit on it) would be to do everything we know to avoid inflammation and, bada bing, bada boom, all problems go away.
But there’s a problem.
Is Inflammation a Cause or Effect?
While there is a clear relationship between all of the above situations, and specifically bipolar, and inflammation there is often a problem of determining cause and effect. So in the case of obesity, is inflammation causing obesity or is obesity causing inflammation?
Could it be that brain inflammation develops first and this causes pathological changes in the brain and this causes other problems which continues to drive obesity or prevent it from being fixable? Because that latter interpretation was the conclusion of one of the papers I linked above where they write
For one, inflammation occurs much more rapidly in the hypothalamus than in peripheral tissues following the switch to an obesogenic HFD, such that it precedes weight gain.
Available data are compatible with a model in which the initial cause of hypothalamic inflammation induced by HFD feeding involves injury to neurons that comprise energy balance neurocircuits. In turn, this injury may undermine homeostatic responses that protect against weight gain, thereby contributing to obesity pathogenesis.
Admittedly based on animal studies (which don’t always translate to humans), what they are saying is that a high calorie high fat diet causes the brain to become inflamed which might damage circuits involved in food regulation which leads to obesity which leads to peripheral inflammation which might serve to sustain the problem (this is seen in other aspects of obesity). Overeating drives brain inflammation which causes weight gain which causes peripheral inflammation.
The same could be occurring in bipolar but as of 2016, cause and effect haven’t been determined that I can tell.
As a major review points out:
The direction of causation has yet to be established; however, the temporal relation- ship of BD and inflammatory conditions suggests that the interaction between BD, inflammation, and medical comorbidities is likely bidirectional. Inflammation may be a common cause to both BD and medical comorbidity.
Alternatively, medical comorbidity may induce an inflammatory state, thus increasing the risk of developing BD or vice versa. Indeed, BD may predate an inflammatory comorbidity, the comor- bidity may predate the onset of BD, or both may have a similar time of onset. There- fore, the direction of causality remains unclear.
Disease states might cause inflammation which puts someone at risk for bipolar or an episode, or bipolar may be causing inflammation in the brain which causes other problems in the body which trigger inflammation which might then work to maintain the bipolar.
I’d also note that it’s been known for a while that bipolar cycles tend to get worse with each progressive cycle and overtime and it could also be that the inflammatory response to a given episode causes changes in the immune system that predisposes the system to become more easily inflamed later.
This is testable but has not yet been tested. I’d note that there are other mechanisms, not the least of which is potentially a loss of cells in the brain. Basically, there may be progressive damage occurring with every cycle. As the same paper states
Each mood episode may induce the neuro- progression of disease, facilitating decreased neural circuit function in key brain regions subserving cognition. With each stepwise decline in cognition, a new lower baseline may be established.
This proposed decline in cognition secondary to inflammation and mood ep- isodes in bipolar disorder (BD) has yet to be fully established; however, it presents as a test- able hypothesis of interest.
Certainly avoiding extremely inflammatory states with proper diet, regular exercise, etc. can’t hurt but to conclude that inflammation is causing bipolar is a little bit preliminary so far as I’m concerned. The correlation of bipolar with inflammation simply can’t provide information on the direction of causation. Yes they are causally related but we don’t yet know if a bipolar episode causes inflammation or whether inflammation kicks off the episode or whether one triggers the other which maintains the problem.
Testing this in humans would be difficult although it could be tested in one of two ways. One would be to artificially generate inflammation (i.e. inject an inflammatory compound) and this has been shown to trigger depression.
Another would be to track bipolar individuals over time to see if something causing inflammation (i.e. stress or sickness) occurs before a bipolar episode. But at this time all that’s been done is to examine bipolar individuals during an episode and noting increased amounts of inflammation. But this doesn’t show causality or even whether or not brain or peripheral inflammation is occurring first.
Finally, I find it interesting that almost all of the above seems to be related only to the depressive aspect of bipolar but not mania and I think determining why this might be may be important going forwards. Since it’s often a cyclical disease, it’s a little bit hard to tell whether the mania or depression is occurring ‘first’ in the cycle.
If the inflammation is only related to the depression, then what’s going on with the manic part of the disease? Is there some aspect of mania that causes the inflammation to go away? Or could the effect of mania be to kick off the inflammatory state that causes the depression. I don’t know and nobody else does either right now.
So the long answer to a short question: yes, bipolar (and likely other mental illness) is related to inflammation but nobody is quite sure how yet. There is a central (brain) and peripheral (body) aspect but which is driving the bus is unclear. For now. Which isn’t in any way to say that reducing inflammation in an overall sense is necessarily a bad thing but rather that I find that some of the conclusions I’ve seen drawn in this regard may be a bit preliminary.
Time will tell.
Facebook Comments